The Canadian SCAD Study
The Canadian SCAD study investigated the risk factors and outcomes of spontaneous coronary artery dissection (SCAD). This prospective observational study enrolled 750 non-atherosclerotic SCAD patients from 22 cardiac centers in North America.
More than 85% of the patients were treated conservatively. The reported in-hospital mortality was as low as 0.1%, while the reported major adverse cardiovascular events (MACE) rate was 8.8%, implying that SCAD patients require close monitoring.
Dr. Jacqueline Saw, Professor at the University of British Columbia commented on the results of the study saying,“Our study supports the fact that first-line therapy for SCAD should be conservative management and PCI should be limited to patients at high risk with ongoing chest pain, ischemia, or patients who are hemodynamically unstable such as those with cardiogenic shock, ventricular tachycardia, ventricular fibrillation and left main dissection.”
“Our study supports the fact that first-line therapy for SCAD should be conservative management and PCI should be limited to patients at high risk with ongoing chest pain, ischemia, or patients who are hemodynamically unstable such as those with cardiogenic shock, ventricular tachycardia, ventricular fibrillation and left main dissection.”- Dr. Jacqueline Saw, M.D.
Insights from the French TAVI registry
The study published in the Journal of American College of Cardiology investigated the optimal anti-thrombotic treatment after transcatheter aortic valve replacement (TAVR) by studying the independent correlates of long-term all-cause mortality and early bioprosthetic valve dysfunction (BVD).
The study concluded that male gender, chronic renal failure, and atrial fibrillation were strongly correlated with a higher all-cause mortality at 3 years. It was also found that anti-coagulant administration at the time of discharge and non-femoral approach decreased the risk of BVD after TAVR.
Dr. Jean Phillipe Collet, the head of the Action Study Group remarked, “The major question that remains unanswered is whether anti-coagulation itself is detrimental or whether it is because of the indication. The missing link is between bioprosthetic valve dysfunction and mortality or stroke, and this relationship is yet to be determined.”
“The major question that remains unanswered is whether anticoagulation itself is detrimental or whether it is because of the indication. The missing link is between bioprosthetic valve dysfunction and mortality or stroke, and this relationship is yet to be determined.”- Dr. Jean Phillippe Collet, M.D.
The ASCEND trial
The ASCEND trial investigated the role of aspirin in the primary prevention of cardiovascular events in diabetic patients. About 15,500 diabetic patients with no history of cardiac disease were randomized to either receiving aspirin or placebo.
Aspirin was associated with lower serious cardiac events but this was offset by an increase in major bleeding events. It was also found that there was no difference in the incidence of gastrointestinal tract cancer or all cancers between the two groups.
Dr. Jane Armitage, Professor of Clinical Trials and Epidemiology and The Honorary Consultant in Public Health Medicine said, “We have to bear in mind that we do not want to cause harm. Having said that, the other issue is how do you balance having a major ischemic stroke against having a major bleed? They are not comparable and it becomes a matter of judgment. All we can say is, this is what the data shows.”
“We have to bear in mind that we do not want to cause harm. Having said that, the other issue is how do you balance having a major ischemic stroke against having a major bleed? They are not comparable and it becomes a matter of judgment. All we can say is, this is what the data shows.”- Dr. Jane Armitage, M.D.
Omega-3 fatty acids for cardiovascular prevention
A randomized clinical trial that enrolled 15,500 diabetic patients assessed the role of omega-3 fatty acids in the primary prevention of cardiovascular disease. The investigators found no significant difference in the risk of serious cardiovascular events in those administered omega−3 fatty acids as compared to placebo. Patients were randomized in a 1:1 ratio to either receive omega-3 fatty acids or placebo, and were observed for the occurrence of a primary outcome of serious cardiovascular events (a composite of non-fatal myocardial infarction, stroke, transient ischemic attack, or vascular death, excluding confirmed intracranial hemorrhage) or a secondary outcome of serious vascular event or any arterial revascularization.
There was no significant difference in the rates of primary or secondary outcomes. Dr. Louise Bowman, Professor at the University of Oxford said, “Our study population was extremely well treated in terms of cardiovascular risk factors. About three-fourths of patients were on a statin, the majority of them were on anti-hypertensives, and diabetes was well controlled. In the context of all of those cardiovascular protective agents, the added benefit of other items such as omega- 3 fatty acids may as well be limited.”
“Our study population was extremely well treated in terms of cardiovascular risk factors. About three-fourths of patients were on a statin, the majority of them were on antihypertensives, and diabetes was well controlled. In the context of all of those cardiovascular protective agents, the added benefit of other items such as omega- 3 fatty acids may as well be limited.”- Dr. Louise Bowman, M.D.
REDUCE LAP HF-1
In this phase 2, double-blinded, randomized controlled trial, the safety of interatrial shunt device (IASD; Corvia Medical) in patients with heart failure (HF) with preserved ejection fraction (an ejection fraction of 40% or above) was assessed as compared to a sham-control arm (femoral venous access with intracardiac echocardiography but no IASD placement).
The safety was assessed by looking into the major adverse cardiac, cerebrovascular, or renal events (MACCRE). After 12 months, there was no significant difference in the rates of MACCRE between the groups. Other outcomes assessed were HF hospitalizations, New York Heart Association (NYHA) Class, quality of life, a 6-minute walk test and device patency.
There was no significant difference in MACCRE rate between the groups with no strokes reported. Moreover, the shunts were found to be patent in all the patients in the IASD group. An improvement in the rate of HF hospitalization and NYHA class was observed in the IASD group but it did not reach statistical significance. There was no difference in the quality of life and 6-minute walk test among patients assigned to both arms of the study.
The lead author, Dr. Ted Feldman, who is an interventional cardiologist at NorthShore University Health-Evanston Hospital commented “Altogether, we have a pilot trial with 11 patients, non-randomized study with 64 patients and 22 patients treated in the randomized group. When we look at all of them, it is pretty clear that we have demonstrated both mechanistically, that these exercise wedge pressures diminish and that the various clinical indications are all favorable.”
“Altogether, we have a pilot trial with 11 patients, non-randomized study with 64 patients and 22 patients treated in the randomized group. When we look at all of them, it is pretty clear that we have demonstrated both mechanistically, that these exercise wedge pressures diminish and that the various clinical indications are all favorable.”- Dr. Ted Feldman, M.D.
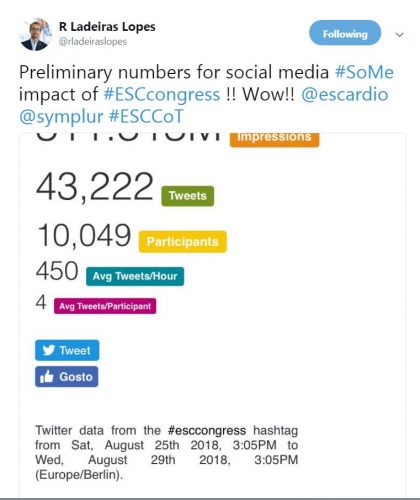
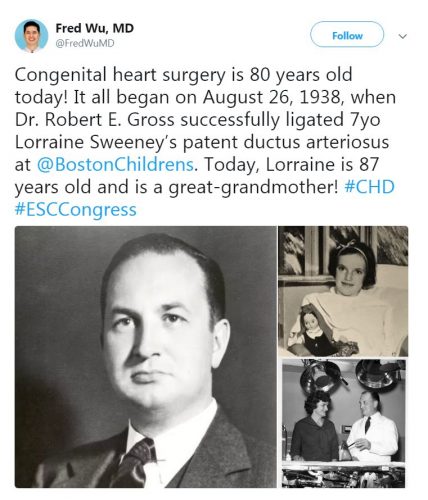
Comments from the social media



Leave a Reply
You must be logged in to post a comment.